
Experts in autocracies have pointed out that it is, unfortunately, easy to slip into normalizing the tyrant, hence it is important to hang on to outrage. These incidents which seem to call for the efforts of the Greek Furies (Erinyes) to come and deal with them will, I hope, help with that. As a reminder, though no one really knows how many there were supposed to be, the three names we have are Alecto, Megaera, and Tisiphone. These roughly translate as “unceasing,” “grudging,” and “vengeful destruction.”
My primary care physiocian once told me I deserved an honorary medical degree because I can spell all my prescription drugs (proprietary and generic), as well as all my OTC meds (proprietary and generic) correctly. He was joking, of course. I simply was born with the spelling gene, and I also do my best to pay attention. But his remark does illustrate how little attention so many people pay to matters of their own health. I am not a doctor nor a medical technician, and I certainly don’t play one on TV. But I do do “due diligence” when anythong new turns up in or near my own body (near meaning physically near, like a pandemic, or emotionally near, like in one or more people I care about.) And cancer is something none of us can really avoid being near at some point or other. So when something like this turns up, so does my gaze.
==============================================================
‘Masked’ cancer drug stealthily trains immune system to kill tumors while sparing healthy tissues, reducing treatment side effects
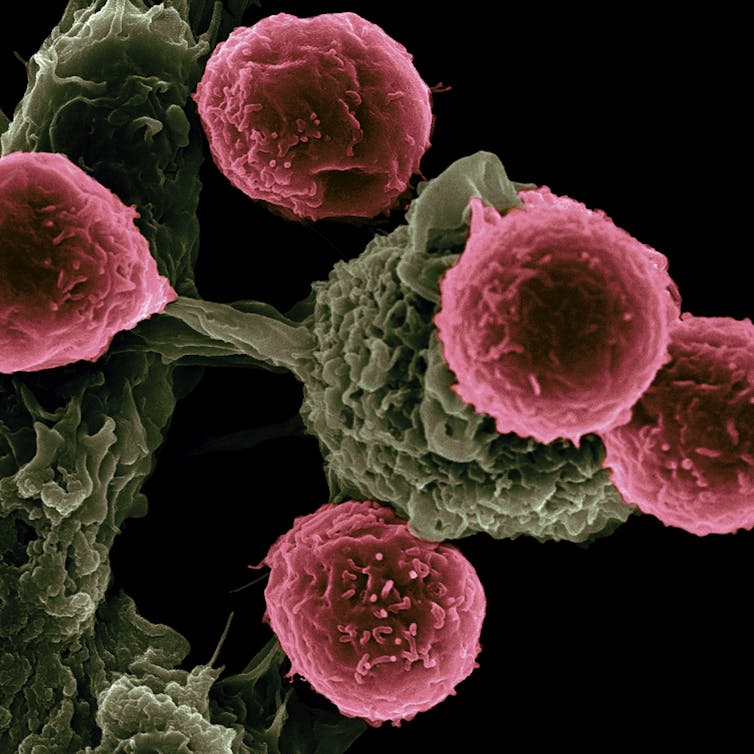
Victor Segura Ibarra and Rita Serda/National Cancer Institute via Flickr, CC BY-NC
Aslan Mansurov, University of Chicago Pritzker School of Molecular Engineering
Many cancer treatments are notoriously savage on the body. Drugs often attack both healthy cells and tumor cells, causing a plethora of side effects. Immunotherapies that help the immune system recognize and attack cancer cells are no different. Though they have prolonged the lives of countless patients, they work in only a subset of patients. One study found that fewer than 30% of breast cancer patients respond to one of the most common forms of immunotherapy.
But what if drugs could be engineered to attack only tumor cells and spare the rest of the body? To that end, my colleagues and I at the University of Chicago’s Pritzker School of Molecular Engineering have designed a method to keep one promising cancer drug from wreaking havoc by “masking” it until it reaches a tumor.
The promise of IL-12
Cytokines are proteins that can modulate how the immune system responds to threats. One way they do this is by activating killer T cells, a type of white blood cells that can attack cancer cells. Because cytokines can train the immune system to kill tumors, this makes them very promising as cancer treatments.
One such cytokine is interleukin-12, or IL-12. Though it was discovered more than 30 years ago, IL-12 still isn’t an FDA-approved therapy for cancer patients because of its severe side effects, such as liver damage. This is in part because IL-12 instructs immune cells to produce a large amount of inflammatory molecules that can damage the body.
Scientists have since been working to reengineer IL-12 to be more tolerable while retaining its powerful cancer-killing effects.
Masking the killer
To create a safer version of IL-12, my colleagues and I took advantage of one of the main differences between healthy and cancerous tissue: an excess of growth-promoting enzymes in cancers. Because cancer cells proliferate very rapidly, they overproduce certain enzymes that help them invade the nearby healthy tissue and metastasize to other parts of the body. Healthy cells grow at a much slower pace and produce fewer of these enzymes.
With this in mind, we “masked” IL-12 with a cap that covers the part of the molecule that normally binds to immune cells to activate them. The cap is removed only when it comes into contact with enzymes found in the vicinity of tumors. When these enzymes chop off the cap, IL-12 is reactivated and spurs nearby killer T cells to attack the tumor.
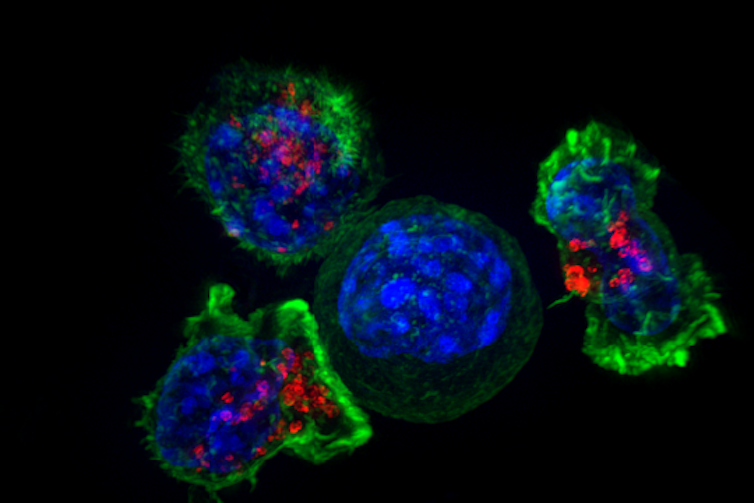
NIH/Flickr
When we applied these masked IL-12 molecules to both healthy and tumor tissue donated by melanoma and breast cancer patients, our results confirmed that only the tumor samples were able to remove the cap. This indicated that masked IL-12 could potentially drive a strong immune response against tumors without causing damage to healthy organs.
We then examined how safe masked IL-12 is by measuring liver damage biomarkers in mice. We found that immune-related side effects typically associated with IL-12 were notably absent in mice treated with masked IL-12 over a period of several weeks, indicating improved safety.
In breast cancer models, our masked IL-12 resulted in a 90% cure rate, while treatment with a commonly used immunotherapy called a checkpoint inhibitor resulted in only a 10% cure rate. In a model of colon cancer, masked IL-12 showed a 100% cure rate.
Our next step is to test the modified IL-12 in cancer patients. While it will take time to bring this encouraging development directly to patients, we believe a promising new treatment is on the horizon.![]()
Aslan Mansurov, Postdoctoral Researcher in Molecular Engineering, University of Chicago Pritzker School of Molecular Engineering
This article is republished from The Conversation under a Creative Commons license. Read the original article.
==============================================================
Alecto, Megaera, and Tisiphone, “training” certainly implies a lower level of intellectual involvement than “teaching” or “educating,” but even so, it sounds like pure science fiction to even think about “training”a non-sentient particle such as a protein to act in a certain way – to stop working in some environments and start working in others. Even though it accomplishes this mission by reacting in a particular way to particular enzymes, it still sounds virtually miraculous. This solution is not ready to approve yet, but it is ready for testing in live cancer patients, and, though I know it will take time, I am looking forward to seeing resutlts from that testing. Please, Eumenides, keep an eye out (and help in any way you can.)
The Furies and I will be back.

